Abstract
Background
Anxiety and depression can seriously undermine mental health and quality of life globally. The consumption of junk foods, including ultra-processed foods, fast foods, unhealthy snacks, and sugar-sweetened beverages, has been linked to mental health. The aim of this study is to use the published literature to evaluate how junk food consumption may be associated with mental health disorders in adults.
Methods
A systematic search was conducted up to July 2023 across international databases including PubMed/Medline, ISI Web of Science, Scopus, Cochrane, Google Scholar, and EMBASE. Data extraction and quality assessment were performed by two independent reviewers. Heterogeneity across studies was assessed using the I2 statistic and chi-square-based Q-test. A random/fixed effect meta-analysis was conducted to pool odds ratios (ORs) and hazard ratios (HRs).
Results
Of the 1745 retrieved articles, 17 studies with 159,885 participants were suitable for inclusion in the systematic review and meta-analysis (seven longitudinal, nine cross-sectional and one case-control studies). Quantitative synthesis based on cross-sectional studies showed that junk food consumption increases the odds of having stress and depression (OR = 1.15, 95% CI: 1.06 to 1.23). Moreover, pooling results of cohort studies showed that junk food consumption is associated with a 16% increment in the odds of developing mental health problems (OR = 1.16, 95% CI: 1.07 to 1.24).
Conclusion
Meta-analysis revealed that consumption of junk foods was associated with an increased hazard of developing depression. Increased consumption of junk food has heightened the odds of depression and psychological stress being experienced in adult populations.
Keywords: Junk food, Mental health, Stress, Depression
Background
Psychological conditions such as bipolar affective disorder, eating disorders, anxiety disorders, and depressive disorders impose a considerable burden across the international community, adversely affecting quality of life [1, 2]. Psychological problems including depression, stress, and anxiety, also arise in association with some non-communicable diseases including cardiovascular disease (CVD), stroke, and cancer [3]. All of these mental health problems have adverse effects on health status, quality of life, and ability to work [4].
Genetics, socioeconomic status, exercise habits, diet, and nutritional status, are understood to be key contributors to the development of emotional or behavioral problems [5]. Food-mood relationships underpin well-known pathways, suggesting that unhealthy eating habits and poor nutritional status are correlated with various mental health problems and behavioral disturbances in adults [6]. This infers that mood and psychological health may be influenced by nutritional habits [7].
The world-wide consumption of junk foods, which include ultra-processed foods, fast foods, unhealthy snacks, and sugar-sweetened beverages, is increasing. The hallmarks of junk foods are that they have high levels of energy, fat, sugar, and salt, accompanied by low levels of micronutrients, fiber, and other bioactive compounds [8]. The low nutritional value of junk foods can alter inflammatory pathways, leading to an increase in biomarkers for oxidative stress and inflammation, which contribute to biological changes associated with mental health disorders. In vitro studies have demonstrated that junk food consumption can negatively affect the brain and mental health [9, 10].
However, the findings of epidemiological studies are inconsistent. Some studies showed the significant association between junk foods consumption and mental health disorders. However, other studies did not mention any relationship [4, 11, 12]. The aim of this study is to examine the relationship between junk food consumption and mental health disorders in adults by conducting a systematic review and meta-analysis of published studies to date.
Methods
The current systematic review and meta-analysis study was conducted according to the PRISMA 2020 statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [13, 14], included studies assessing the relationship between junk food consumption and mental health in adults.
Search strategy
A systematic literature search was conducted in PubMed/Medline, ISI Web of Science, Scopus, Cochrane, Google Scholar, and EMBASE up to July 2023. The following keywords were used in this search: “sweetened drink*” OR “sweetened beverage*” OR snack* OR “processed food*” OR “junk food*” OR “soft drinks” OR “sugared beverages” OR “fried foods” OR “instant foods” OR sweets for junk food consumption and “mental health” OR depression OR stress OR anxiety OR “sleep dissatisfaction” OR “sleep disorders” OR happiness OR wellbeing for mental health status. In PubMed, keywords were searched through [tiab] and [MeSH] tags. Articles were required to be written in English language; there was no limitation regarding the year of publication. The reference lists of included papers were also examined to avoid missing other published data.
Inclusion and exclusion criteria
Two investigators independently screened the articles retrieved during the literature search. Publications that fulfilled the following criteria were eligible for inclusion: (1) observational studies that were conducted in adults (cohort, case-control, cross-sectional); and (2) studies that examined the relationship between junk food consumption and mental health status. We excluded letters, comments, reviews, meta-analyses, ecological, in vitro, and pre-clinical studies, as well as duplicate studies.
Data extraction
For each eligible study, the following information was extracted: first author, year of publication, study design, country, age range, gender, sample size, type of junk food, dietary assessment tool, mental health parameters, mental health assessment tool, study quality score, effect sizes and measures, and covariates.
It should be noted that in the present study, junk food intake was considered using four categories: (i) sweet drinks (fruit-flavored drinks, sweetened coffee, fruit juice drinks, sugared coffee and tea, energy drinks, cola drinks, beverages, soft drinks, lemonade, and soda), (ii) sweet snacks (total sugars, added sugars, sweetened desserts, fatty/sweet products, ice cream, chocolate, artificial sweeteners, sweet snacks, dessert, sauces and dressings, candy, patterns of consumption of sweet, high fat and sugary foods, biscuits and pastries, cakes, pie/cookies, and baked goods), (iii) snacks (including snacks, sauces/added fats, fast food, fast-food pattern, western diet pattern, snacking and convenience pattern, fried foods, fried potato, crisps, salty snacks, convenience pattern, instant foods), and (iv) total junk foods (all types of junk foods).
Quality assessment of studies
The quality of the included studies was examined using the Newcastle-Ottawa Scale (NOS) [15, 16]. The NOS assigns a maximum of 9 points to each study: 4 for selection, 2 for comparability, and 3 for assessment of outcomes (for cohort study) or exposures (for case-control study).
The maximum score for cohort and case-control studies were 9 and for cross-sectional studies were 7. In the current analysis, the quality of studies is defined good if the studies get 3 or 4 stars in the selection domain AND 1 or 2 stars in the comparability domain AND 2 or 3 stars in the outcome/exposure domain. Besides, fair quality is defined as 2 stars in the selection domain AND 1 or 2 stars in the comparability domain AND 2 or 3 stars in the outcome/exposure domain and finally, poor quality is defined for 0 or 1 star in the selection domain OR 0 star in the comparability domain OR 0 or 1 star in the outcome/exposure domain.
All steps including searching, article screening, data extraction, and quality assessment of articles were independently performed by two investigators. Disagreements between the two investigators were resolved by discussion to reach consensus.
Statistical analysis
The results of the current quantitative synthesis are presented as hazard ratios (HRs) or odds ratios (ORs) and 95% confidence intervals (95% CI). STATA version 14.0 (StataCorp, College Station, TX) software was used to perform the meta-analysis. We conducted meta-analysis whenever at least two studies investigated similar associations between junk food consumption and mental health problems.
I2 statistic and chi-square-based Q-test were used for the assessment of heterogeneity. In the current study, a lack of heterogeneity was inferred when the p-value of chi-square-based Q-test exceeded 0.10. Fixed models were used to pool HRs and ORs when the heterogeneity p-value was higher than 0.10. Random models were used to pool the ORs whenever the heterogeneity p-value was equal to or less than 0.10, followed by Galbraith analysis and sensitivity analysis. Subgroup analysis was also conducted to identify the source of heterogeneity. Publication bias was measured using Begg’s test or Egger’s test and considered substantial whenever the resulting p-value was < 0.1.
Results
Systematic search results
The flow diagram for the process of study selection is shown in the PRISMA flowchart (Fig. 1). Based on the initial search, we found 1745 papers. After removal of duplicate documents and title and abstract screening, 69 articles remained for more detailed assessment. Full texts of these papers were reviewed carefully by three researchers, with 17 articles satisfying the eligibility requirements for inclusion in the systematic review and meta-analysis.
Fig. 1.
The PRISMA flowchart for the process of study selection
Characteristics of the included studies
Seventeen studies evaluating a total of 159,885 participants were included in our quantitative synthesis. A considerable number of participants were female, with seven articles restricted to female participants. Most of the included studies were cross-sectional (58.82%), with the remaining seven (47.05%) being cohort studies. It should be noted that Reinks et al. (2013) presented both cross-sectional and longitudinal data. Reinks et al. (2013) and ten other papers (64.70% in total) assessed depression as an outcome. Nine (52.94%) of studies assessed anxiety or stress as outcomes. In terms of dietary exposures, various types of junk foods such as ultra-processed food, beverages, and snacks were evaluated across the 17 studies. Table 1 illustrates detailed characteristics of records including the age of participants and provenance of studies. All of the included studies have good quality.
Table 1.
Characteristics of the included studies
| Number | Author/ (year) | Study characteristics | Psychological outcomes | Dietary exposures | QA | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Design | Provenance | Sample size | Age (range or mean) |
Male Gender n (%) |
psychological condition | Assessment tool | Type of junk food | Assessment tool (Practical definition) |
||||
| 1 | Adjibade, 2019 | Cohort | France | 26,730 | 47.26 ± 14.17 | 6350 (23.75) | Depression |
CES-D (0–60) validated cut-offs (CES-D score ≥ 17 for men and ≥ 23 for women) |
Ultra-processed food |
Manufactured food products containing numerous ingredients as well as additives such as hydrogenated oils, non-sugar sweeteners, modified starch, flavoring agents, emulsifiers, humectants, colors, and other additives used for cosmetic purpose measured based on web-based dietary record platform validated for self-administration |
7 | |
|
Beverages, fatty/sweet products, snacks, and sauces/ added fats |
Percentage of dietary intake based on a web-based dietary record platform validated for self-administration | |||||||||||
| 2 | Almajwal, 2016 | cross-sectional | Saudi Arabia | 395 | NR | 0 (0.0) | Stress | The perceived stress scale |
Eating styles including, Restrained, Emotional, and External |
The Dutch Eating Behavior Questionnaire self-reported questionnaire. | 6 | |
| Eating fast food |
frequency of eating fast food per week |
|||||||||||
| 3 | Camiller, 2014 | Cohort | France | 30,240 | 46.2 ± 13.9 | 7378 (24.40) | Depressive symptoms | Validated French version of the Center for Epidemiologic Studies Depression Scale (CES-D) | Sugar-sweetened soft drinks | French version of the revised 21-item Three-Factor Eating Questionnaire | 7 | |
| 4 | Canuto, 2021 | cross-sectional | Brazil | 539 | 33.6 ± 8.6 | 0 (0.0) | Perceived stress score | 10-item Perceived Stress Scale (PSS-10) | Snack and fast-food | Validated qualitative food frequency questionnaire comprising 53 food items | 8 | |
| 5 | Chaplin, 2011 | Cross sectional | United Kingdom | 870 | 45 | 75 (8.62) |
Stress in life in general, work stress, cognitive failure outside work, minor injury outside work, and minor injury at work |
Researcher-made validated questionnaire | Unhealthy snack | A factor analysis of snacking behavior, consisted of the sum of frequency of snacking of chocolate, crisps and biscuits, measured using a Likert scale | 6 | |
| 6 | Coletro, 2022 | Cross-sectional | Brazil | 1693 | NR | 827 (48.9) | Anxiety symptoms | The Generalized Anxiety Disorder 7-item (GAD-7) | consumption of ultra-processed foods |
Assessed using a qualitative food frequency questionnaire (FFQ), validated in Brazilian population referring to consumption in the last 3 months |
7 | |
| Depression symptoms | Patient Health Questionnaire-9 (PHQ-9) | |||||||||||
| 7 | Crawford, 2011 | Cross sectional | United States | 626 | 45–54 | 0 (0.0) | Depression | The Center for Epidemiological Studies-Depression (CES-D) scale (scoring 16 or higher out of 20 items) | Fast food |
Frequency of fast-food intake was measured by self-report |
7 | |
| 8 | Gómez-Donoso, 2019 | Cohort | Spain | 14,907 | 36.7 ± 11.7 | 0 (0.0) | Depression | Clinical diagnosis or antidepressant medication use | Ultra-processed food | Frequency of intake of carbonated drinks, processed meat, biscuits (cookies), candy (confectionery), ‘instant’ packaged soups and noodles, sweet or savory packaged snacks, and sugared milk and fruit drinks | 7 | |
| 9 | Le Port, 2012 | cohort | France | 12,404 |
M:45.0 ± 2.9 F: 42.2 ± 4.2 |
9272 (74.75) | Depression | The 20 items scale of The Center for Epidemiological Studies-Depression (CES-D) |
Western diet, fat-sweet, snacking, and dessert |
35-item qualitative Food Frequency Questionnaire (FFQ) for twenty food groups | 8 | |
| 10 | Lim, 2020 | longitudinal study | United States | 912 | 28.7 ± 0.3 | 0 (0.0) | Chronic stress | 10-item Perceived Stress Scale (PSS-10) | Excess fat and soda intake | Frequency of intake of instant noodle, frozen, canned or microwave foods, potato chips, corn chips and tortilla chips, McDonald’s, KFC, Pizza Hut/Bi Sheng Ke | 7 | |
| 11 | Liu, 2007 | Cross sectional | China | 2541 | 20.4 | 1470 (57.85) | Stress | 10-item Perceived Stress Scale (PSS-10) | Ready to eat food or snack | Not validated food frequency questionnaire regarding the previous month | 6 | |
| Depression score | The 20 items scale of The Center for Epidemiological Studies-Depression (CES-D) | |||||||||||
| 12 | Nitturi, 2021 | Cross sectional | United States | 107 | 49.3 ± 11.6 | 22 (20.56) | Anxiety sensitivity | The Anxiety Sensitivity Index (ASI) | Unhealthy Supersized fast food | Researcher-made validated questionnaire | 7 | |
| 13 | Rienks, 2013 | Longitudinal and cross-sectional data driven from a prospective study | Australia | 8369 for cross-sectional and 6060 for longitudinal analysis | 50–55 | 0 (0.0) | Depression | The 10-items scale of Centre for Epidemiologic Studies Depression (scores ranges from 0–30, participants with a score of 10 or higher were considered depressed | Meat and processed meat and high fat and sugar pattern | validated food frequency questionnaire asking regarding 74 foods and six alcoholic beverages over the last 12 months | 8 | |
| 14 | Sangsefidi, 2020 |
Cross-sectional (Data from The recruitment phase of a cohort) |
Iran | 9965 | 20–69 | 4921 (49.7) |
Depression, Anxiety, and Stress |
The Iranian validated version of depression, anxiety, and stress scale questionnaire 21 (DASS 21), a well-known short version of self-report |
Sweetened drinks, Fast foods, Canned foods, Fried foods, and Snacks |
Not validated Food Frequency Questionnaire (FFQ), asking about the last year (results were divided into three groups of never, once, or more than once per week) |
7 | |
| 15 | Sousa, 2013 | Cross sectional | Brazil | 46,785 | 20–59 | 22,410 (47.9) | Depression | Patient Health Questionnaire-9 (PHQ-9) |
Sugar sweetened beverage, Sweets, and Snacks |
Not validated Food Frequency Questionnaire (FFQ), asking about the last week (High consumption was considered when a participant reported 5 times or more intake per week) |
7 | |
| 16 | Xia, 2017 | Case control | China | 2702 |
Control:45.84 Case: 46.08 |
1450 (53.66) | depression | Chinese version of Zung Self-Rating Depression Scale (SDS) |
Sugared beverages, Salted foods |
Not validated food frequency questionnaire (FFQ), consisted of 81 items, including 7 frequency categories ranging from “almost never eat” to “twice or more per day” | 7 | |
| 17 | Zenk, 2014 | Prospective cohort | United States | 100 | 44.3 ± 10.5 | 0 (0.0) |
Stressful events, within-person stressful social interaction, and between-person stressful social interaction |
Researcher-made not validated questionnaire | Snack food intake | Not validated web-based momentary surveys via study provided smartphones | 6 | |
F, Females; M, Males; NR, Not Reported
Qualitative synthesis
Most of the included studies concordantly showed at least a single significant link between junk food consumption and psychological outcomes. This was despite their use of different measures of association, dissimilar exposure duration and outcomes, and heterogenous definitions, all of which made it challenging to draw conclusions from the qualitative synthesis (summarized in Table 2). Nevertheless, findings from some studies were discordant. For instance, while Sangsefidi et al. (2020) and Chaplin et al. (2011) demonstrated a significant association between stress and snack intake, Almajwal et al. (2016) and Zenk et al. (2014) reported non-significant findings, despite the use of similar measures of association and comparable adjustments for covariates. Although a notable number of studies showed a significant link between junk food intake and psychological disorders, the level of disagreement across studies meant that a meta-analysis was essential in order to clarify this relationship.
Table 2.
Findings of qualitative synthesis
| NO | Author/ (year) | Psychological outcomes | Dietary exposures | Measure of association | Study findings | Confounders | ||
|---|---|---|---|---|---|---|---|---|
| 1 | Adjibade, 2019 | Depression | Ultra-processed food (Q4/Q1) | HR (95% CI) | 1.29 (1.13–1.47)* | Age, sex, BMI, marital status, education, occupational categories, household income per consumption unit, residential area, number of 24-h dietary records, inclusion month, energy intake without alcohol, alcohol intake, smoking, PA, dietary patterns, intakes of lipids, sodium, and carbohydrates. | ||
| Beverages (Q4/Q1) | 1.25 (1.13–1.38)* |
Age, sex, marital status, educational level, occupational categories, household income per consumption unit, residential area, energy intake without alcohol, number of 24-h dietary records, inclusion month, smoking status, physical activity, BMI, health events during follow-up (cancer, type 2 diabetes, hypertension and cardiovascular events) and quantity of the equivalent food group. |
||||||
| Fatty/sweet products (Q4/Q1) | 1.08 (0.96–1.22) | |||||||
| Snacks (Q4/Q1) | 1.10 (0.98–1.24) | |||||||
| Sauces/ added fats (Q4/Q1) | 1.23 (1.10–1.39) | |||||||
| 2 | Almajwal, 2016 | Stress | Eating styles | Restrained | Spearman’s correlation coefficients | 0.115 | p-value < 0.05 | Age, gender, education, experience, and marital status |
| Emotional | 0.128 | |||||||
| External | 0.170 | |||||||
| Stress (low vs. high) | Eating fast food (low) | Never or rarely | Number of participants (Chi-square) | 42 (18.7) | χ2 = 14.99; p = 0.002 | Not adjusted | ||
| Sometimes | 169 (75.1) | |||||||
| Often | 9 (4.0) | |||||||
| Almost everyday | 5 (2.2) | |||||||
| Eating fast food (high) | Never or rarely | 29 (13.7) | ||||||
| Sometimes | 145 (68.7) | |||||||
| Often | 29 (13.7) | |||||||
| Almost everyday | 8 (3.8) | |||||||
| Eating snacks (low) | Never or rarely | 28 (12.4) | χ2 = 0.43; p = 0.934 | |||||
| Sometimes | 147 (65.3) | |||||||
| Often | 37 (16.4) | |||||||
| Almost everyday | 13 (5.8) | |||||||
| Eating snacks (high) | Never or rarely | 28 (13.3) | ||||||
| Sometimes | 141 (66.8) | |||||||
| Often | 32 (15.2) | |||||||
| Almost everyday | 10 (4.7) | |||||||
| 3 | Camilleri, 2014 | Depressive symptoms | Sugar-sweetened soft drinks | OR (95% CI) | Male | 1.02 (0.72, 1.44) * | Age, total daily energy intake, BMI, educational level, employment status, marital status, smoking status, physical activity, history of dieting, and season of completing the 24-h records | |
| Female | 1.03 (0.83–1.27) * | |||||||
| 4 | Canuto, 2021 | Perceived stress score | snack and fast-food | PR (95% CI) | 1.28 (1.04–1.56) * | Age, skin color, marital status, education, BMI, wake time and work shift | ||
| 5 | Chaplin, 2011 | Stress in life in general | Unhealthy snack | OR (95% CI) | 1.57 (1.15–2.16) * | Smoking, alcohol, sleep problems, age, sex, breakfast frequency, exposure to physical hazards and working hours score, Demand- control- support score, and Effort-Reward imbalance score. | ||
| Work stress | 1.61 (1.13–2.29) * | |||||||
| Cognitive failure outside work | 1.51 (1.07–2.12)* | |||||||
| Minor injury outside work | 1.54 (1.14–2.09)* | |||||||
| Minor injury at work | 1.95 (1.40–2.71)* | |||||||
| 6 | Coletro, 2022 | Anxiety symptoms | consumption of ultra-processed foods | PR (95% CI) | 1.5 (1.03–2.3) * |
Sex, age, marital status, educational background, family income and medical diagnosis of depression or anxiety disorders |
||
| Depression symptoms | 1.5 (1.1–2.1) * | |||||||
| 7 | Crawford, 2011 | Depression (present/ absent) | Fast food | OR (95% CI) | F: 1.54 (1.06–2.25)* | Age, race, marital status, education, annual household income, BMI, smoking, leisure PA, alcohol use, ADD. | ||
| 8 | Gómez-Donoso, 2019 | Depression (incidence) | Ultra-processed food (Q4/Q1) | HR (95% CI) | 1.33 (1.07–1.64)* | Sex, age, year, baseline BMI, total energy intake, PA, smoking, marital status, living alone, employment status, working hours per week, health-related career, years of education, adherence to Trichopoulou’s MeDiet Score, baseline self-perception of competitiveness, anxiety, dependence levels. | ||
| 9 | Le Port, 2012 | Depression | Western diet (Q4/Q1) | OR (95% CI) | M: 1.36 (1.19–1.54)* | Age, employment position at 35, professional activity, BMI, marital status, PA, tobacco, smoking, alcohol intake. | ||
| Fat-sweet (Q4/Q1) | M: 1.49 (1.30–1.71)* | |||||||
| Snacking (Q4/Q1) |
M: 1.50 (1.32–1.71)* F: 1.43 (1.16–1.76)* |
|||||||
| Dessert (Q4/Q1) | F: 1.03 (0.84–1.26) | |||||||
| 10 | Lim, 2020 | Chronic stress (yes/ no) | Excess fat/ soda intake | PR (95% CI) | 1.39 (1.05–1.84)* | Demographic characteristics, total dietary calorie intake. | ||
| 11 | Liu, 2007 | Perceived stress score | Ready to eat food (low/ high frequency) | OR (95% CI) | 0.69 (0.57–0.84)* | Sex, city, perceived weight, smoking. | ||
| Snack food (low/ high frequency) | 0.75 (0.59–0.94)* | |||||||
| Depression score | Snack food (low/ high frequency) | 0.73 (0.58–0.93)* | - | |||||
| Ready to eat food (low/ high frequency) | 0.70 (0.57–0.86)* | Sex, grade, city, perceived weight, smoking, alcohol use. | ||||||
| Fast food (low/ high frequency) | 0.40 (0.12–1.37)* | |||||||
| 12 | Nitturi, 2021 | Anxiety sensitivity | Unhealthy/Supersized fast food (always/ never) | OR (95% CI) | 1.05 (1.01–1.08)* | Sex, age, and BMI | ||
| 13 | Rienks, 2013 | Prevalence of depression | Meat and processed meat | OR (95% CI) | 1.06 (0.99–1.13) | Energy, smoking, PA, ability to manage on available income, occupation status, education, marital status, mean stress score, BMI category. | ||
| High fat and sugar pattern | 1.02 (0.96–1.09) | |||||||
| Incidence of depression | Meat and processed meat | 1.09 (0.98–1.21) | ||||||
| High fat and sugar pattern | 1.08 (0.96–1.20) | |||||||
| 14 | Sangsefidi, 2020 | Depression | Sweetened drinks (never/ Once or more per week) | OR (95% CI) | 0.76 (0.59–0.96)* | Age, education level, PA, history of chronic diseases, smoking and BMI | ||
| Anxiety | 0.76 (0.62–0.93)* | |||||||
| Stress | 0.63 (0.48–0.82)* | |||||||
| Depression | Fast foods (never/ Once or more per week) | 1.61 (1.18–2.203)* | ||||||
| Anxiety | 1.19 (0.908–1.56) | |||||||
| Stress | 1.28 (0.88–1.86) | |||||||
| Depression | Canned foods (never/ Once or more per week) | 1.12 (0.78–1.61) | ||||||
| Anxiety | 1.13 (0.83–1.54) | |||||||
| Stress | 1.05 (0.69–1.59) | |||||||
| Depression | Fried foods (never/ Once or more per week) | 1.03 (0.69–1.52) | ||||||
| Anxiety | 1.01 (0.73–1.39) | |||||||
| Stress | 2.47 (1.46–4.18)* | |||||||
| Depression | Snacks (never/ Once or more per week) | 1.36 (1.01–1.84)* | ||||||
| Anxiety | 1.99 (1.55–2.56)* | |||||||
| Stress | 1.73 (1.23–2.45)* | |||||||
| 15 | Sousa, 2013 | Depression | Sugar sweetened beverage (regular/no) | OR (95% CI) | 1.13 (0.99–1.29) | Age, sex, race/color, education, living with spouse, PA, alcohol consumption, tobacco use. | ||
| Sweets (regular/no) | 1.53 (1.33–1.76)* | |||||||
| Snacks (regular/no) | 1.52 (1.21–1.90)* | |||||||
| 16 | Xia, 2017 | Depression | Sugared beverages | OR (95% CI) | 1.09 (0.87, 1.35) | For other food groups intake | ||
| Salted foods | 1.13 (0.90, 1.41) | |||||||
| 17 | Zenk, 2014 | Stressful event | Snack food intake | OR (95% CI) | 1.24 (0.97, 1.60) |
Age, education (high school diploma, GED, or less; associate’s degree or some college; bachelor’s degree; graduate or professional degree), employment status (unemployed/other including retired or Disabled; employed part-time, employed full-time), annual per capita household income (approximate tertiles: <$7500, $7500-18,749, ≥$18,750), automobile ownership, and body mass index (BMI), calculated as interviewer-measured weight (kg/[height (m)]2) |
||
| Within-person stressful social interaction | 0.90 (0.67, 1.22) | |||||||
| Between-person stressful social interaction | 1.10 (1.00, 1.22) | |||||||
Abbreviations SES: socioeconomic status, ST: screen time, NR: not reported, ADHD: Attention deficit hyperactivity disorder, T: tertile, Q: quantile, PA: Physical Activity, ADD: use of anti-depressive drugs, CF: cognitive function, OR: odds ratio, RR: relative risk, HR: hazard ration, SMD: standardized mean difference
Quantitative synthesis
Pooling OR in cross-sectional studies
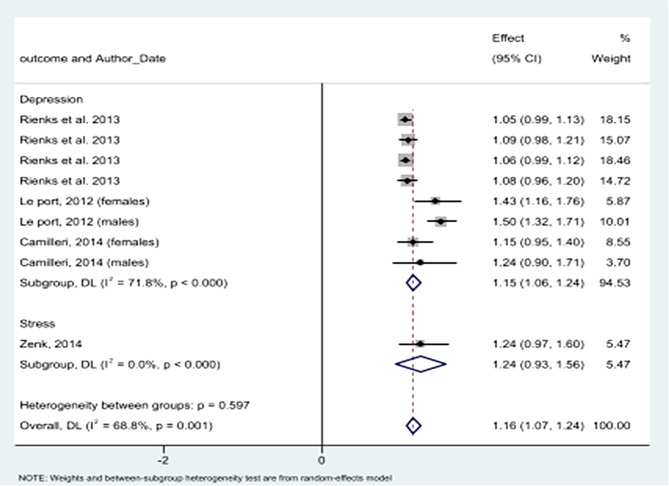
Four cross-sectional studies (n = 13,500) demonstrated that junk food consumption was associated with increased stress (pooled OR = 1.33, 95% CI: 1.02 to 1.65). This finding shows a significant association; however, a notable level of heterogeneity was observed (I² = 74.3%, p = 0.009) (Fig. 2; Table 3). Also, six cross-sectional studies, including 74,127 participants, illustrated a significant association between junk food consumption and depression, with a pooled OR of 1.16 (95% CI: 1.04 to 1.28) (Fig. 2). Overall, junk food consumption indicated a significant association with increased odds of mental health problems (OR = 1.15, 95% CI: 1.06 to 1.23). The Egger’s test for small-study effects indicated evidence of publication bias (p > 0.001). To address this bias, a trim and fill analysis was conducted, resulting in an adjusted OR of 1.11 (95% CI: 0.95 to 1.30). Funnel plot is presented in Fig. 3.
Fig. 2.
Junk food consumption (unhealthy snacks and sweetened beverages) and odds of having depression and stress in cross-sectional studies
Table 3.
Findings of Quantitative Synthesis
| No | Study Type | Measure of Association | Outcome | Number of Studies | Sample Size | Pooled Results Measure (95%CI) |
Heterogeneity | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Chi-Squared | I2 | p-value | Model | |||||||
| 1 | Cross-sectional | OR | Stress | 4 | 13,500 | 1.333 (1.018 to 1.649) | 11.68 | 74.3% | 0.009 | Random Effects |
| 2 | Depression | 6 | 74,127 | 1.161 (1.039 to 1.283) | 14.72 | 66.0% | 0.012 | Random Effects | ||
| 3 |
Mental Disorder (Overall) |
10 | 87,627 | 1.148 (1.065 to 1.232) | 27.26 | 67.0% | 0.001 | Random Effects | ||
| 4 |
Mental Disorder (After trim and fill) |
15 | 87,627 | 1.11 (0.95–1.30) | N/A | N/A | N/A | Random Effects | ||
| 5 | PR | Stress | 2 | 2,232 | 1.312 (1.071–1.552) | 0.39 | 0.0% | 0.530 | Fixed | |
| 6 | Cohorts | OR | Depression | 8 | 46,821 | 1.152 (1.062–1.241) | 24.81 | 71.8% | 0.001 | Random |
| 7 |
Mental Disorder (Overall) |
9 | 46,921 | 1.156 (1.070–1.242) | 25.66 | 68.8% | 0.001 | Random | ||
| 8 | HR | Depression | 2 | 41,637 | 1.300 (1.154 to 1.446) | 0.06 | 0.0% | 0.813 | Fixed | |
CI, Confidence Interval; OR, Odds Ratio; PR, Prevalence Ratio; HR, Hazard Ratio
Fig. 3.
Funnel plot, using data from cross-sectional studies investigating the association between junk food consumption and mental health problems
Pooling PR in cross-sectional studies
Two cross-sectional studies focusing on stress with a combined sample size of 2,232 participants reported a PR of 1.31 (95% CI: 1.07–1.55) (Fig. 4).
Fig. 4.
Association between junk foods consumption and having stress in cross-sectional studies
Pooling OR in cohort studies
Pooling results of cohort studies showed that junk food consumption significantly increases the odds of depression by 15% (OR = 1.15; 95% CI: 1.06 to 1.24). After inclusion of the single cohort study that considered stress as its outcome, the overall OR of junk foods consumption and mental disorders was 1.16 (OR = 1.16, 95% CI: 1.07 to 1.24) (Fig. 5).
Fig. 5.
Association between junk foods consumption and having mental health problems in cohort studies
Although Egger’s test for small-study effects yielded a bias coefficient of 2.53, standard error of 1.19, and a p-value of 0.07, trim and fill analysis did not impute any studies, and the overall OR remained unchanged. Figure 6 demonstrates the funnel plot.
Fig. 6.
Funnel plot, using data from cohort studies investigating the association between junk food consumption and mental health problems
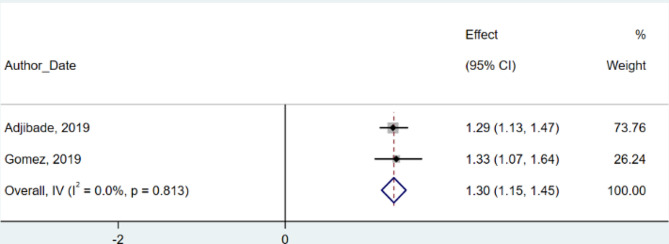
Pooling HR in cohort studies
Aggregating two cohort studies with 41,637 participants showed an HR of 1.30 (95% CI: 1.15 to 1.45) for depression, demonstrating a significant risk increase (Fig. 7). Remarkably, these studies showed no heterogeneity (I² = 0.0%, p = 0.81) or publication bias.
Fig. 7.
Junk food consumption and risk of depression in cohort studies
Discussion
The meta-analysis reported in the present study showed that high consumption of junk foods was significantly associated with increased risks of depression. In addition, higher junk food consumption was associated with increased odds of depression and psychological stress. This association between consumption of food with low nutritional value and mental health was demonstrated in multiple studies on different populations and cultures [17–19].
Meta-analysis of prospective studies showed that increased risk of subsequent depression and adverse mental health outcomes were correlated with higher ultra-processed food intake [20]. According to meta analysis incorporating seven studies, junk food consumption increased the risk of experiencing mental illness symptoms [21]. For example, one study reporting outcomes for 1591 adults, demonstrated that high consumption of fast foods and processed foods was associated with anxiety, nervousness, restlessness, lack of motivation and depressive symptoms [22]. In another study, weight gain due to unhealthy eating was associated with deterioration in mental health in 404 adults during the second year of the COVID-19 pandemic [23]. Our findings are consistent with a recent systematic review and dose-response meta-analysis that included 26 studies and 260,385 participants from twelve countries, which showed that ultra-processed food consumption increased risk of depression [24].
Epidemiological data suggests that unhealthy food consumption may be associated with poorer mental health through its adverse effects on inflammatory processes, nutritional status, and neurotransmitter function. Inflammation has previously been associated with underlying biological bases for depression [25]. Several observational and meta-analysis studies have demonstrated an inverse association between the consumption of healthy foods including vegetables, fruits, whole-grain and fish, with depressive symptoms [26–29]. Healthy dietary patterns include a significant amount of tryptophan, an essential amino acid and precursor to serotonin; evidence shows that reduction in the availability of serotonin is associated with depression [30, 31].
The adoption of western dietary patterns that regularly include junk foods and fast foods can increase the probability of developing inflammatory and cardiovascular diseases. Inflammatory conditions are related to mental health disorders including depression, stress and anxiety [32, 33]. In addition, life stressors may augment the interconnection between depressive mood and unhealthy dietary patterns through activation of the brain’s reward system by foods that are high in sugar, fat, and salt [34].
There is also evidence that brain-derived neurotrophic factor (BDNF) may be reduced by consumption of a high fat diet. BDNF is associated with supporting existing neurons and the production of new neurons and implicated in the pathogenesis of depressive disorder. A reduction in BDNF impairs synaptic and cognitive function and neuronal growth, contributing to the development of psychological disorders [35]. Western-type diets include a higher amount of polyunsaturated omega-6 fatty acids, which increase proinflammatory eicosanoids, and decrease BDNF and neuronal membrane fluidity [36]. This suggests that the adverse effects of junk and fast foods on mental health might be associated with the high content of unhealthy fats contained in these foods [4]. Moreover, intake of high amounts of sugar through consumption of sweet drinks and snacks can lead to endothelial dysfunction, inflammation, and exaggerated insulin production that may also influence mood [37–40].
Mood disorder may itself influence diet, with some studies reporting that patients with depression consume a large amount of carbohydrate-fat-rich foods during their depressive episodes [41–43]. Serotonin, an important neurotransmitter for regulating mood, may play a prominent role in this respect given that the sole source of its precursor, tryptophan, is through the diet [44].
The consumption of ultra-processed foods is positively correlated with unhealthy eating habits, including lower intake of fruits and vegetables and higher intake of sweet foods or beverages [8, 45]. It is notable that ultra-processed foods contain additives as well as molecules that are generated by high-temperature heating. These can alter gut microbiota composition and reduce nutrient absorption [46]. Some studies have explored the association between the gut microbiome and mental health [47–49], with animal studies suggesting that food additives might increase symptoms of and susceptibility to anxiety and depression via changes of gut microbiota composition [50, 51].
The present paper found that the outcomes of studies selected for the meta-analysis were not always in agreement. This may have been due to confounding factors such as past history of depression or negative life events not being included in the analysis, differences in study designs, sample sizes or population characteristics, non-homogeneous assessment of dietary patterns, and inconsistencies in the evaluation of psychological disorders including the use of different diagnostic criteria to define mental health status.
On the other side, some studies have reported that mental health disorders including depression and psychological stress may reduce an individual’s motivation to eat healthy foods and sometime lead to overeating [17], skipping main meals and replacing them with high calories foods [30]. Some individuals consume high energy and fatty foods during stressful situations, choosing these more palatable foods as an unconscious or deliberate strategy to change their energy levels and mood [52, 53]. Stress affects neuroendocrine function by activating the hypothalamic-pituitary-adrenal (HPA) axis, increasing the secretion of glucocorticoids. These change glucose metabolism, promote insulin resistance, and alter the secretion of appetite-related hormones. All of these factors contribute to the propensity to eat more high-calorie palatable food [12]. However, there are also studies that report no differences in eating patterns under stressful and non-stressful conditions [54, 55]. The analysis presented in the present study cannot be used to demonstrate causality. On the basis of the evidence, it is plausible that there is a bidirectional relationship between junk food consumption and mental health [17]. It remains unclear whether the quality of food choices affects susceptibility to poorer mental health outcomes, and/or the experience of unpleasant emotions influences the quality of food selection [30]. Evidence for a causal pathway is unclear and needs to be further investigated in well-controlled longitudinal studies. Our meta-analysis on cross-sectional studies showed an association between junk food consumption and increased odds of having stress and depression. Besides, meta-analysis on cohort studies demonstrated that junk foods consumption increases the risk of developing stress and depression.
Strengths and limitations
As the main strength of our study, we have comprehensively and specifically evaluated earlier findings regarding the association between junk food consumption and mental health status in adults. The present study has some limitations arising from the studies selected for meta-analysis. Inconsistencies in design of studies such as the ways that diet is assessed using different dietary questionnaire tools, the influence of seasonal and hormonal variations of depressive symptoms, and the use of different diagnostic criteria for defining mental health status is one of the limitations of this study. Despite the association shown between consumption of junk foods and mental health disorders, the strength of the associations and number of documents included in this study is unable to demonstrate causality.
Conclusion
The present study supports the conclusion that consumption of junk foods that are high in fat and sugar content and of low nutritive value are associated with poorer mental health in adults. Further studies utilizing a longitudinal design are needed to better determine the directionality and effect size of junk food consumption on psychological disorders. Moreover, more studies are warranted to assess the mechanisms involved in this relationship to provide scientific support for changes in public health policies.
Acknowledgements
We would like to thank Dr. Jillian Broadbear for their invaluable contribution in editing and reviewing this manuscript.
Author contributions
H.E: conception and design of the study, acquisition and analysis of data, drafting the manuscript, P.M: quality assessment and drafting the manuscript, B.H: screening and data extraction, FS.M: data extraction and drafting the manuscript, BG: data extraction and quality assessment, K.G: data extraction and analysis of data, M.HB: conception and design of the study, drafting the manuscript, M.Q: conception and design of the study, analysis of data and drafting the manuscript.
Funding
The authors gratefully acknowledge funding provided by the Alborz University of Medical Sciences.
Data availability
Data will be made available on request from the authors.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Motahar Heidari-Beni, Email: heidari.motahar@gmail.com.
Mostafa Qorbani, Email: mqorbani1379@yahoo.com, Email: mqorbani1379@gmail.com.
References
- 1.Connell J, Brazier J, O’Cathain A, Lloyd-Jones M, Paisley S. Quality of life of people with mental health problems: a synthesis of qualitative research. Health Qual Life Outcomes. 2012;10:138. doi: 10.1186/1477-7525-10-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arias D, Saxena S, Verguet S. Quantifying the global burden of mental disorders and their economic value. EClinicalMedicine. 2022;54:101675. doi: 10.1016/j.eclinm.2022.101675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khaustova OO, Markova MV, Driuchenko MO, Burdeinyi AO. Proactive psychological and psychiatric support of patients with chronic non-communicable diseases in a randomised trial: a Ukrainian experience. Gen Psychiatr. 2022;35(5):e100881. doi: 10.1136/gpsych-2022-100881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sangsefidi ZS, Lorzadeh E, Hosseinzadeh M, Mirzaei M. Dietary habits and psychological disorders in a large sample of Iranian adults: a population-based study. Ann Gen Psychiatry. 2020;19:8. doi: 10.1186/s12991-020-00263-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gu Y, Zhu Y, Xu G. Factors associated with mental health outcomes among health care workers in the Fangcang shelter hospital in China. Int J Soc Psychiatry. 2022;68(1):64–72. doi: 10.1177/0020764020975805. [DOI] [PubMed] [Google Scholar]
- 6.El Ansari W, Adetunji H, Oskrochi R. Food and mental health: relationship between food and perceived stress and depressive symptoms among university students in the United Kingdom. Cent Eur J Public Health. 2014;22(2):90–7. doi: 10.21101/cejph.a3941. [DOI] [PubMed] [Google Scholar]
- 7.Tuck NJ, Farrow C, Thomas JM. Assessing the effects of vegetable consumption on the psychological health of healthy adults: a systematic review of prospective research. Am J Clin Nutr. 2019;110(1):196–211. doi: 10.1093/ajcn/nqz080. [DOI] [PubMed] [Google Scholar]
- 8.Adjibade M, Julia C, Allès B, Touvier M, Lemogne C, Srour B, et al. Prospective association between ultra-processed food consumption and incident depressive symptoms in the French NutriNet-Santé cohort. BMC Med. 2019;17(1):78. doi: 10.1186/s12916-019-1312-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hahad O, Prochaska JH, Daiber A, Muenzel T. Environmental noise-Induced effects on stress hormones, oxidative stress, and vascular dysfunction: key factors in the relationship between Cerebrocardiovascular and Psychological disorders. Oxid Med Cell Longev. 2019;2019:4623109. doi: 10.1155/2019/4623109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adnan M, Chy MNU, Kamal A, Chowdhury KAA, Rahman MA, Reza A et al. Intervention in Neuropsychiatric disorders by suppressing inflammatory and Oxidative Stress Signal and Exploration of in Silico studies for potential lead compounds from Holigarna Caustica (Dennst.) Oken leaves. Biomolecules. 2020;10(4). [DOI] [PMC free article] [PubMed]
- 11.Xia Y, Wang N, Yu B, Zhang Q, Liu L, Meng G, et al. Dietary patterns are associated with depressive symptoms among Chinese adults: a case-control study with propensity score matching. Eur J Nutr. 2017;56(8):2577–87. doi: 10.1007/s00394-016-1293-y. [DOI] [PubMed] [Google Scholar]
- 12.Canuto R, Garcez A, Spritzer PM, Olinto MTA. Associations of perceived stress and salivary cortisol with the snack and fast-food dietary pattern in women shift workers. Stress. 2021;24(6):763–71. doi: 10.1080/10253890.2021.1919615. [DOI] [PubMed] [Google Scholar]
- 13.Hasani H, Mardi S, Shakerian S, Taherzadeh-Ghahfarokhi N, Mardi P. The novel coronavirus disease (COVID-19): a PRISMA systematic review and meta-analysis of clinical and paraclinical characteristics. Biomed Res Int. 2020;2020:1–16. doi: 10.1155/2020/3149020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, et al. PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst Reviews. 2021;10(1):1–19. doi: 10.1186/s13643-020-01542-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. Newcastle-Ottawa quality assessment scale cohort studies. University of Ottawa; 2014.
- 16.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 17.Crawford GB, Khedkar A, Flaws JA, Sorkin JD, Gallicchio L. Depressive symptoms and self-reported fast-food intake in midlife women. Prev Med. 2011;52(3–4):254–7. doi: 10.1016/j.ypmed.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rossa-Roccor V, Richardson CG, Murphy RA, Gadermann AM. The association between diet and mental health and wellbeing in young adults within a biopsychosocial framework. PLoS ONE. 2021;16(6):e0252358. doi: 10.1371/journal.pone.0252358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van der Velde LA, Zitman FM, Mackenbach JD, Numans ME, Kiefte-de Jong JC. The interplay between fast-food outlet exposure, household food insecurity and diet quality in disadvantaged districts. Public Health Nutr. 2022;25(1):105–13. doi: 10.1017/S1368980020004280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lane MM, Gamage E, Travica N, Dissanayaka T, Ashtree DN, Gauci S, et al. Ultra-processed food consumption and mental health: a systematic review and meta-analysis of observational studies. Nutrients. 2022;14(13):2568. doi: 10.3390/nu14132568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hafizurrachman M, Hartono RK. Junk food consumption and symptoms of mental health problems: a meta-analysis for public health awareness. Kesmas: Jurnal Kesehatan Masyarakat Nasional. (Natl Public Health Journal). 2021;16(1).
- 22.Rosenberg L, Welch M, Dempsey G, Colabelli M, Kumarasivam T, Moser L et al. Fast foods, and Processed Foods May worsen perceived stress and Mental Health. FASEB J. 2022;36.
- 23.Almandoz JP, Xie L, Schellinger JN, Mathew MS, Marroquin EM, Murvelashvili N, et al. Changes in body weight, health behaviors, and mental health in adults with obesity during the COVID-19 pandemic. Obesity. 2022;30(9):1875–86. doi: 10.1002/oby.23501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mazloomi SN, Talebi S, Mehrabani S, Bagheri R, Ghavami A, Zarpoosh M et al. The association of ultra-processed food consumption with adult mental health disorders: a systematic review and dose-response meta-analysis of 260,385 participants. Nutr Neurosci. 2022:1–19. [DOI] [PubMed]
- 25.Coletro HN, Mendonça RD, Meireles AL, Machado-Coelho GLL, Menezes MC. Ultra-processed and fresh food consumption and symptoms of anxiety and depression during the COVID – 19 pandemic: COVID inconfidentes. Clin Nutr ESPEN. 2022;47:206–14. doi: 10.1016/j.clnesp.2021.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li Y, Lv MR, Wei YJ, Sun L, Zhang JX, Zhang HG, et al. Dietary patterns and depression risk: a meta-analysis. Psychiatry Res. 2017;253:373–82. doi: 10.1016/j.psychres.2017.04.020. [DOI] [PubMed] [Google Scholar]
- 27.Hodge A, Almeida OP, English DR, Giles GG, Flicker L. Patterns of dietary intake and psychological distress in older australians: benefits not just from a Mediterranean diet. Int Psychogeriatr. 2013;25(3):456–66. doi: 10.1017/S1041610212001986. [DOI] [PubMed] [Google Scholar]
- 28.Mihrshahi S, Dobson AJ, Mishra GD. Fruit and vegetable consumption and prevalence and incidence of depressive symptoms in mid-age women: results from the Australian longitudinal study on women’s health. Eur J Clin Nutr. 2015;69(5):585–91. doi: 10.1038/ejcn.2014.222. [DOI] [PubMed] [Google Scholar]
- 29.Nguyen B, Ding D, Mihrshahi S. Fruit and vegetable consumption and psychological distress: cross-sectional and longitudinal analyses based on a large Australian sample. BMJ Open. 2017;7(3):e014201. doi: 10.1136/bmjopen-2016-014201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu C, Xie B, Chou CP, Koprowski C, Zhou D, Palmer P, et al. Perceived stress, depression and food consumption frequency in the college students of China Seven cities. Physiol Behav. 2007;92(4):748–54. doi: 10.1016/j.physbeh.2007.05.068. [DOI] [PubMed] [Google Scholar]
- 31.Rienks J, Dobson AJ, Mishra GD. Mediterranean dietary pattern and prevalence and incidence of depressive symptoms in mid-aged women: results from a large community-based prospective study. Eur J Clin Nutr. 2013;67(1):75–82. doi: 10.1038/ejcn.2012.193. [DOI] [PubMed] [Google Scholar]
- 32.Khosravi M, Sotoudeh G, Majdzadeh R, Nejati S, Darabi S, Raisi F, et al. Healthy and unhealthy dietary patterns are related to Depression: a case-control study. Psychiatry Investig. 2015;12(4):434–42. doi: 10.4306/pi.2015.12.4.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khosravi M, Sotoudeh G, Amini M, Raisi F, Mansoori A, Hosseinzadeh M. The relationship between dietary patterns and depression mediated by serum levels of folate and vitamin B12. BMC Psychiatry. 2020;20(1):63. doi: 10.1186/s12888-020-2455-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Le Port A, Gueguen A, Kesse-Guyot E, Melchior M, Lemogne C, Nabi H, et al. Association between dietary patterns and depressive symptoms over time: a 10-year follow-up study of the GAZEL cohort. PLoS ONE. 2012;7(12):e51593. doi: 10.1371/journal.pone.0051593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miao Z, Wang Y, Sun Z. The relationships between stress, Mental disorders, and epigenetic regulation of BDNF. Int J Mol Sci. 2020;21(4). [DOI] [PMC free article] [PubMed]
- 36.Shakya PR, Melaku YA, Page A, Gill TK. Association between dietary patterns and adult depression symptoms based on principal component analysis, reduced-rank regression and partial least-squares. Clin Nutr. 2020;39(9):2811–23. doi: 10.1016/j.clnu.2019.12.011. [DOI] [PubMed] [Google Scholar]
- 37.Bishwajit G, O’Leary DP, Ghosh S, Sanni Y, Shangfeng T, Zhanchun F. Association between depression and fruit and vegetable consumption among adults in South Asia. BMC Psychiatry. 2017;17(1):15. doi: 10.1186/s12888-017-1198-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kingsbury M, Dupuis G, Jacka F, Roy-Gagnon MH, McMartin SE, Colman I. Associations between fruit and vegetable consumption and depressive symptoms: evidence from a national Canadian longitudinal survey. J Epidemiol Commun Health. 2016;70(2):155–61. doi: 10.1136/jech-2015-205858. [DOI] [PubMed] [Google Scholar]
- 39.Hamer M, Chida Y. Associations of very high C-reactive protein concentration with psychosocial and cardiovascular risk factors in an ageing population. Atherosclerosis. 2009;206(2):599–603. doi: 10.1016/j.atherosclerosis.2009.02.032. [DOI] [PubMed] [Google Scholar]
- 40.Sousa KT, Marques ES, Levy RB, Azeredo CM. Food consumption and depression among Brazilian adults: results from the Brazilian National Health Survey, 2013. Cadernos De Saude Publica. 2019;36(1):e00245818. doi: 10.1590/0102-311x00245818. [DOI] [PubMed] [Google Scholar]
- 41.Daneshzad E, Keshavarz SA, Qorbani M, Larijani B, Azadbakht L. Association between a low-carbohydrate diet and sleep status, depression, anxiety, and stress score. J Sci Food Agric. 2020;100(7):2946–52. doi: 10.1002/jsfa.10322. [DOI] [PubMed] [Google Scholar]
- 42.Włodarczyk A, Cubała WJ, Stawicki M. Ketogenic diet for depression: A potential dietary regimen to maintain euthymia? Progress in neuro-psychopharmacology & biological psychiatry. 2021;109:110257. [DOI] [PubMed]
- 43.Sangsefidi ZS, Salehi-Abarghouei A, Sangsefidi ZS, Mirzaei M, Hosseinzadeh M. The relation between low carbohydrate diet score and psychological disorders among Iranian adults. Nutr Metabolism. 2021;18(1):16. doi: 10.1186/s12986-021-00546-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moncrieff J, Cooper RE, Stockmann T, Amendola S, Hengartner MP, Horowitz MA. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry. 2022. [DOI] [PMC free article] [PubMed]
- 45.Lee J, Allen J. Gender Differences in Healthy and Unhealthy Food Consumption and its relationship with Depression in Young Adulthood. Commun Ment Health J. 2021;57(5):898–909. doi: 10.1007/s10597-020-00672-x. [DOI] [PubMed] [Google Scholar]
- 46.Roca-Saavedra P, Mendez-Vilabrille V, Miranda JM, Nebot C, Cardelle-Cobas A, Franco CM, et al. Food additives, contaminants and other minor components: effects on human gut microbiota-a review. J Physiol Biochem. 2018;74(1):69–83. doi: 10.1007/s13105-017-0564-2. [DOI] [PubMed] [Google Scholar]
- 47.Simkin DR. Microbiome and Mental Health, specifically as it relates to adolescents. Curr Psychiatry Rep. 2019;21(9):93. doi: 10.1007/s11920-019-1075-3. [DOI] [PubMed] [Google Scholar]
- 48.Järbrink-Sehgal E, Andreasson A. The gut microbiota and mental health in adults. Curr Opin Neurobiol. 2020;62:102–14. doi: 10.1016/j.conb.2020.01.016. [DOI] [PubMed] [Google Scholar]
- 49.Dickerson F, Dilmore AH, Godoy-Vitorino F, Nguyen TT, Paulus M, Pinto-Tomas AA et al. The Microbiome and Mental Health Across the Lifespan. Current topics in behavioral neurosciences. 2022. [DOI] [PubMed]
- 50.Quines CB, Rosa SG, Da Rocha JT, Gai BM, Bortolatto CF, Duarte MM, et al. Monosodium glutamate, a food additive, induces depressive-like and anxiogenic-like behaviors in young rats. Life Sci. 2014;107(1–2):27–31. doi: 10.1016/j.lfs.2014.04.032. [DOI] [PubMed] [Google Scholar]
- 51.Campos-Sepúlveda AE, Martínez Enríquez ME, Rodríguez Arellanes R, Peláez LE, Rodríguez Amézquita AL, Cadena Razo A. Neonatal monosodium glutamate administration increases aminooxyacetic acid (AOA) susceptibility effects in adult mice. Proceedings of the Western Pharmacology Society. 2009;52:72 – 4. [PubMed]
- 52.Choi J. Impact of stress levels on eating behaviors among College Students. Nutrients. 2020;12(5). [DOI] [PMC free article] [PubMed]
- 53.Radavelli-Bagatini S, Sim M, Blekkenhorst LC, Bondonno NP, Bondonno CP, Woodman R, et al. Associations of specific types of fruit and vegetables with perceived stress in adults: the AusDiab study. Eur J Nutr. 2022;61(6):2929–38. doi: 10.1007/s00394-022-02848-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bellisle F, Louis-Sylvestre J, Linet N, Rocaboy B, Dalle B, Cheneau F, et al. Anxiety and food intake in men. Psychosom Med. 1990;52(4):452–7. doi: 10.1097/00006842-199007000-00007. [DOI] [PubMed] [Google Scholar]
- 55.Pollard TM, Steptoe A, Canaan L, Davies GJ, Wardle J. Effects of academic examination stress on eating behavior and blood lipid levels. Int J Behav Med. 1995;2(4):299–320. doi: 10.1207/s15327558ijbm0204_2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request from the authors.