Abstract
Coronary heart disease (CHD) incidence and mortality remain very low in Japan despite major dietary changes and increases in CHD risk factors that should have resulted in substantial increase in CHD rates (Japanese paradox). Primary genetic effects are unlikely, given the substantial increase in CHD in migrant Japanese to the U.S. For men aged 40–49, levels of total cholesterol and blood pressure have been similar in Japan and the U.S. throughout their lifetime. The authors tested the hypothesis that levels of subclinical atherosclerosis, coronary artery calcification and intima-media thickness of the carotid artery (IMT), in men aged 40–49 are similar in Japan and the U.S. The authors conducted a population-based study of 493 randomly-selected men: 250 men in Kusatsu, Shiga, Japan, and 243 white men in Allegheny County, Pennsylvania, U.S. in 2002–2005. The Japanese had a less favorable profile of many risk factors than the whites. Prevalence ratio for the presence of coronary calcium score ≥10 in the Japanese compared to the whites was 0.52 (95% CI, 0.35, 0.76). Mean (SE) IMT was significantly lower in the Japanese (0.616 (0.005) versus 0.672 (0.005) mm, p<0.01). Both associations remained significant after adjusting for risk factors. The findings warrant further investigations.
Keywords: Atherosclerosis, epidemiology, men, risk factors
Coronary heart disease (CHD) mortality in Japan has been uniquely low among industrialized countries (1). This was largely attributed to diet: low intake of saturated fat and cholesterol, resulting in low levels of total cholesterol (TC), e.g., 4.13 mmol/L (160 mg/dL) in Japan versus 6.19 mmol/L (240 mg/dL) in the United States (U.S.) in the 1960s (1). Dietary intake of fat and serum levels of TC have steadily increased with the westernization of lifestyle in Japan (2, 3). CHD mortality in Japan, however, has been decreasing since the 1970s (4). Furthermore, a recent report showed that CHD incidence is much lower in Japan than in other industrialized countries (5). Even in men in the post World-War-II (WWII) birth cohort, who adopted a westernized lifestyle from childhood and young adulthood life, CHD mortality is much lower in Japan than in whites in the U.S. (6). This is despite the fact that TC and blood pressure (BP) have been similar throughout their lifetime between the populations (2, 6–11). Moreover, rates of smoking in this birth cohort have been much higher in the Japanese (2, 11). Careful evaluation of CHD mortality showed that low CHD mortality in men in the post WWII birth cohort in Japan is not due to the misclassification of cause of death (4, 12). Additionally, a recent autopsy study among young men continued to report much lower prevalence of coronary atherosclerosis in the Japanese in Japan than in whites in the U.S. (13). Traditional risk factors for CHD predict CHD in Japanese men similar to the U.S., but at much lower rates of CHD (1, 14). Low CHD in the Japanese is not due to genetics or host susceptibility because CHD incidence and mortality increased substantially in migrants to the U.S. within one to two generations (15, 16). There are three possible reasons for the low CHD mortality in men in Japan: lower amounts of coronary atherosclerosis, reduced amounts of vulnerable plaques given the same amounts of atherosclerosis, and lower prevalence of risk factors related to thrombosis and clinical events.
In this study, we tested the null hypothesis that among men aged 40–49 from population-based samples, levels of subclinical atherosclerosis are not different between the Japanese in Japan and whites in the U.S. We evaluated subclinical atherosclerosis by coronary artery calcification and intima-media thickness of the carotid artery (IMT).
MATERIALS AND METHODS
Subjects
Participants were population-based samples of 493 randomly-selected men aged 40–49: 250 Japanese men from Kusatsu City, Shiga, Japan, and 243 white men from Allegheny County, Pennsylvania, U.S. Exclusion criteria were 1) clinical cardiovascular disease, 2) type 1 diabetes, 3) cancer except skin cancer in the past two years, 4) renal failure, and 5) genetic familial hyperlipidemias. In Japan, men aged 40–49 living in Kusatsu City were randomly selected, based on the Basic Residents' Register of the city. The Register has information on name, age, and sex of the residents. All Japanese nationals are required by law to register. Each selected man was mailed an invitation to the study to determine whether he was willing to participate. In the U.S., white men aged 40–49 living in Allegheny County were randomly selected, based on the voter registration list. The list has information on name, age, sex, and race of the registered voters. The voter registration list is very complete. Each selected man was mailed an invitation to the study to determine whether he was willing to participate. Participation rates were about 50 percent at both centers.
Informed consent was obtained from all participants. The study was approved by the Institutional Review Boards of Shiga University of Medical Science, Otsu, Japan and University of Pittsburgh, Pittsburgh, U.S.
Study protocol
Body weight and height were measured while the participant was wearing light clothing without shoes. Waist girth was measured at the level of the umbilicus while the participant was standing erect. BP was measured in the right arm of the seated participant after the participant emptied his bladder and sat quietly for five minutes, using an appropriate-sized cuff, with an automated sphygmomanometer (BP-8800, Colin Medical Technology, Komaki, Japan). The average of two measurements was used.
Venipuncture was performed early in the clinic visit after a 12-hour fast. The samples at both centers were shipped on dry ice to University of Pittsburgh. Serum lipids were determined with the standardized methods according to the Centers for Disease Control and Prevention, including TC, low-density-lipoprotein cholesterol (LDL-C), high-density-lipoprotein cholesterol (HDL-C), and triglycerides. Serum glucose was determined using a hexokinase–glucose-6-phosphate-dehydrogenase-enzymatic assay, serum insulin using a radio-immuno assay (Linco Research Inc., St. Charles, US), C-reactive protein (CRP) using a calorimetric-competitive-enzyme-linked-immuno-sorbent assay, and fibrinogen using an automated-clot-rate assay (Diagnostica Stago, Parsippany, U.S.).
A self-administered questionnaire was used to obtain information on demography, smoking habits, alcohol drinking, and other factors. Pack-years were calculated as years of smoking multiplied by the number of cigarettes per day divided by 20. Alcohol drinking was assessed as whether the participant drinks beer, wine, liquor, sake (Japanese rice wine), or other alcoholic beverages with quantity and frequency. Alcohol drinkers were defined as those who drank alcohol ≥two days per week. Ethanol consumption per day was estimated, assuming that concentrations of alcohol were five percent for beer, 12 percent for wine, 40 percent for liquor, and 16 percent for sake. Those who exercised were defined as those who regularly exercised ≥one hour per week.
Hypertension was defined as systolic BP ≥140 mmHg, diastolic BP ≥90 mmHg, or use of anti-hypertensive medications. Diabetes mellitus was defined as fasting serum glucose level ≥7 mmol/L or use of anti-diabetic medications.
Electron-beam computed tomography (EBT)
The scanning was done using a GE-Imatron C150 EBT scanner (GE Medical Systems, South San Francisco, U.S.) at both centers. Scanners were calibrated regularly by technicians following a standardized protocol. Heart scanning was performed following a standardized protocol to obtain 30 to 40 contiguous 3-mm-thick transverse images from the level of the aortic root to the apex of the heart. Images were obtained during maximal breath holding using ECG triggering (60 percent of R-R interval) so that each 100-m-second exposure was obtained during the same phase of the cardiac cycle.
One trained reader at the Cardiovascular Institute, University of Pittsburgh, read the images, using a DICOM (Digital Imaging and Communications in Medicine) workstation and software by AccuImage (AccuImage Diagnostic Corporation, San Francisco, U.S.). The software program implements the widely-accepted Agatston scoring method (17). Coronary artery calcification was considered to be present when three contiguous pixels (area=1 mm2) greater than 130 Hounsfield Units were detected overlying the vessels of interest. A coronary calcium score (CCS) was calculated for each region of interest by multiplying the area of all significant pixels by a grade number (one, two, three, four) indicative of the peak computed tomography number (Hounsfield Unit). The reader was blinded to participant’s characteristics and the study centers. The reproducibility of the EBT scans had an intraclass correlation of 0.98.
IMT
Before the study began, sonographers at both centers received training for carotid scanning at the ultrasound laboratory in Pittsburgh. We applied continuous-quality-assessment programs developed by the laboratory to assure the scanning quality (18). A Toshiba 140A scanner equipped with a 7.5 MHz-linear-array imaging probe was used at both centers. The sonographers scanned the right and left common carotid arteries (CCA), the carotid bulbs, and the internal carotid arteries (ICA). For the CCA segment, both near and far walls were examined 1-cm proximal to the bulb. For the bulb area and ICA, only far walls were examined. The scans were recorded on videotape and sent to the laboratory for scoring.
Trained readers at the laboratory digitized the best image for scoring and then measured the average IMT across 1-cm segments of near and far walls of the CCA and the far wall of the carotid bulb and ICA on both sides. Measurements from each location were then averaged to produce an overall measurement of IMT. The readers were blinded to participant’s characteristics and the study centers. Under continuous-quality-assessment programs, correlation coefficients between sonographers and between readers for average IMT were 0.96 and 0.99, respectively (18).
Statistical analyses
To compare risk factors between the populations, a t-test, the Mann-Whitney U test, or chi-square test was used. To examine associations of CCS with risk factors in each population, subjects were divided into three categories based on CCS: 0, <10 (>0 and <10), and ≥10. To examine associations of IMT with risk factors in each population, subjects were divided into three tertile groups using the same cut-points for both Japanese and white men. A linear trend was used to test a trend across the three groups.
To compare prevalence of coronary artery calcification between the populations, multivariate-adjusted prevalence ratio was calculated (19). Two cut points were used to define the presence of coronary artery calcification: CCS=0 and CCS=10. General-linear-model analyses were performed to calculate multivariate-adjusted IMT. For these analyses, traditional risk factors were entered (Models I), followed by CRP and fibrinogen (Model II), and other factors (Models III).
All p-values were two-tailed. P-value <0.05 was considered as significant. SAS (release 8.02, SAS Inc., Cary, North Carolina) was used for all statistical analyses.
RESULTS
A profile of many risk factors in the Japanese was less favorable than or similar to that in the whites, including BP, TC, LDL-C, triglycerides, glucose, smoking, hypertension, and diabetes (Table 1). Exceptions were BMI, waist girth, HDL-C, insulin, fibrinogen, and CRP. Pack-years and ethanol consumption (median, inter-quartile range) were significantly higher in the Japanese than in the whites; 18.9 (3.0, 30.0) versus 0 (0, 0), respectively, for pack-years (p<0.01) and 14.3 (2.0, 42.5) versus 2.9 (0.9, 16.0), respectively, for ethanol consumption (g/day) (p<0.01).
Table 1.
Characteristics of participants in Kusatsu, Shiga, Japan and Allegheny County, Pennsylvania, U.S. in 2002–2005
| Japanese (n=250) | White (n=243) | p | |
|---|---|---|---|
| Age (years) | 45.2 (2.80) | 45.1 (2.9) | >0.75 |
| BMI (kg/m2) | 23.8 (3.1) | 27.8 (4.1) | <0.01 |
| Waist girth (cm) | 85.3 (8.3) | 98.3 (11.1) | <0.01 |
| SBP (mmHg) | 125.1 (16.4) | 122.9 (11.2) | 0.07 |
| DBP (mmHg) | 76.5 (11.9) | 73.6 (8.5) | <0.01 |
| TC (mmol/L) | 5.66 (0.94) | 5.48 (0.99) | 0.04 |
| LDL-C (mmol/L) | 3.47 (0.92) | 3.49 (0.89) | >0.75 |
| HDL-C (mmol/L) | 1.39 (0.33) | 1.24 (0.33) | <0.01 |
| TG (mmol/L) | 1.55 (1.17, 2.05) | 1.42 (1.04, 2.09) | 0.07 |
| Glu (mmol/L) | 5.88 (0.89) | 5.56 (0.64) | <0.01 |
| Insulin (pmol/L) | 72.2 (31.3) | 105.6 (59.0) | <0.01 |
| Fbg (umol/L) | 7.37 (1.90) | 8.67 (2.07) | <0.01 |
| CRP (mg/L) | 0.32 (0.15, 0.67) | 0.87 (0.49, 1.83) | <0.01 |
| Smoker (%) | 49.2 | 5.3 | <0.01 |
| Drinker (%) | 66.8 | 45.3 | <0.01 |
| Exercise (%) | 26.8 | 73.3 | <0.01 |
| Hypertension (%) | 26.4 | 15.2 | <0.01 |
| HT meds (%) | 4.0 | 8.6 | 0.04 |
| Diabetes (%) | 4.8 | 2.1 | 0.14 |
| DM meds (%) | 1.2 | 0.4 | 0.64 |
| Lipid meds (%) | 3.2 | 11.5 | <0.01 |
BMI: body-mass index, SBP: systolic blood pressure, DBP: diastolic blood pressure, TC: total cholesterol, HDL-C: high-density-lipoprotein cholesterol, LDL-C: low-density-lipoprotein cholesterol, TG: triglycerides, Glu: fasting glucose, Fbg: fibrinogen, CRP: C-reactive protein, HT meds: hypertension medications, DM meds: diabetes medications, Lipids meds: lipid-lowering medications
Smoker was defined as current smoker, drinker as those who drank alcohol ≥two days a week, exercise as those who exercised ≥one hour per week, hypertension as SBP ≥140 mmHg, DBP ≥90 mmHg, or use of anti-hypertensive medications, and diabetes as fasting glucose level ≥7 mmol/L or use of anti-diabetic medications. Those who exercised were defined as those who regularly exercised ≥one hour per week.
Values are expressed as mean (SD) or median (inter-quartile range) for continuous variables.
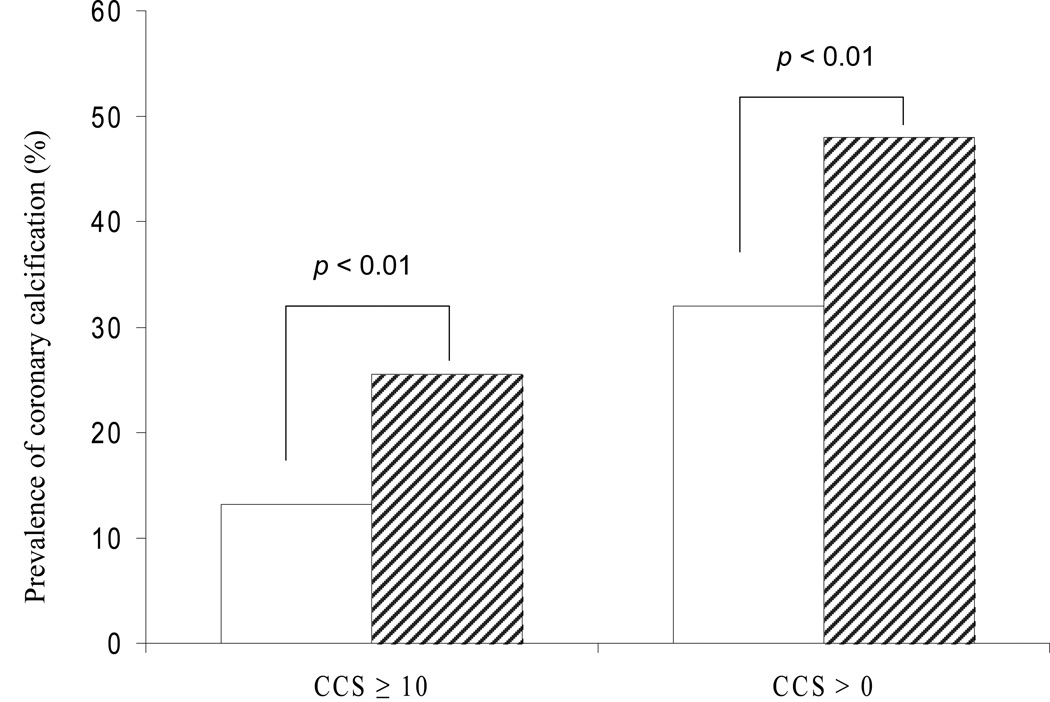
Levels of subclinical atherosclerosis were significantly lower in the Japanese than in the whites. Prevalence of CCS≥10 and CCS>0 was significantly lower in the Japanese than in the whites (Figure 1). The distributions of CCS were skewed in both populations. Among those with CCS>0, 49 (59.8 percent) in the Japanese and 55 (47.0 percent) in the whites showed CCS<10; seven (8.5 percent) in the Japanese and 13 (11.1 percent) in the whites showed CCS≥100. Mean IMT was significantly lower in the Japanese than in the whites: 0.616 (0.005) for the Japanese and 0.672 (0.005) mm for the whites (mean (SE), p<0.01).
Figure 1.
Prevalence of coronary artery calcification (%) in Japanese men aged 40–49 in Kusatsu, Japan and in white men aged 40–49 in Allegheny County, U.S. in 2002–2005
CCS: coronary calcium score
White bars: Japanese, stripped bars: whites
The associations of coronary artery calcification with risk factors were similar between the populations (Table 2). In both populations, the category of CCS was associated with age, BMI, BP, LDL-C, triglycerides, fibrinogen, hypertension, and diabetes. Rates of hypertension were 21.4 percent for those with CCS=0, 40.8 percent for those with CCS<10, and 30.3 percent for those with CCS≥10 in the Japanese (p for trend 0.05), and 10.3, 16.4, and 24.2 percent, respectively, in the whites (p for trend 0.01). Rates of diabetes were 3.6, 6.1 and 9.1 percent, respectively, in the Japanese (p for trend 0.15), and 1.6, 1.8, and 3.2 percent, respectively, in the whites (p for trend 0.48). There was no interaction between risk factors and populations in predicting the category of CCS except for insulin. In the whites levels of insulin were linearly associated with the category of CCS whereas in the Japanese levels of insulin in the category of CCS≥10 were significantly lower than those in the category of CCS<10.
Table 2.
Associations of coronary artery calcification with risk factors in Japanese men aged 40–49 in Kusatsu, Shiga, Japan and in white men aged 40–49 in Allegheny County, Pennsylvania, U.S. in 2002–2005
| Japanese |
Whites |
|||||||
|---|---|---|---|---|---|---|---|---|
| Category of CCS | 0 | <10 | ≥10 | 0 | <10 | ≥10 | ||
| Number (%) | 168 (67%) | 49 (20%) | 33 (13%) | p | 126 (52%) | 55 (23%) | 62 (26%) | p |
| Age (years) | 44.8 (2.9) | 45.6 (2.7) | 46.5 (2.3) | **,§ | 44.7 (2.9) | 44.8 (3.0) | 46.2 (2.6) | **,‡,§ |
| BMI (kg/m2) | 23.1 (2.8) | 25.1 (2.9) | 24.9 (3.7) | **,§ | 26.4 (3.1) | 28.9 (4.6) | 29.4 (4.7) | **,§ |
| SBP (mmHg) | 123.5 (15.1) | 129.2 (18.0) | 127.4 (19.1) | 121.3 (11.0) | 122.5 (11.5) | 126.4 (11.0) | **,§ | |
| DBP (mmHg) | 74.9 (11.3) | 80.4 (12.3) | 78.7 (13.3) | ** | 75.5 (71.7) | 73.9 (8.2) | 77.4 (7.8) | § |
| LDL-C (mmol/L) | 3.39 (0.94) | 3.51 (0.83) | 3.85 (0.86) | **,§ | 3.37 (0.96) | 3.69 (0.83) | 3.57 (0.74) | * |
| HDL-C (mmol/L) | 1.40 (0.33) | 1.33 (0.29) | 1.39 (0.39) | 1.29 (0.35) | 1.21 (0.27) | 1.17 (0.33) | # | |
| TG (mmol/L) | 1.46 (1.06, 1.94) | 1.63 (1.38, 2.39) | 1.64 (1.23, 2.23) | **,§ | 1.28 (0.96, 1.70) | 1.66 (1.10, 1.23) | 1.55 (1.06, 2.16) | *,# |
| Glu (mmol/L) | 5.77 (0.59) | 6.14 (1.48) | 6.05 (0.88) | 5.51 (0.48) | 5.49 (0.56) | 5.72 (0.91) | *,# | |
| Insulin (pmol/L) | 67.4 (28.5) | 88.9 (33.3) | 71.5 (34.7) | † | 90.3 (38.2) | 120.1 (63.9) | 124.3 (77.8) | **,§ |
| Fbg (umol/L) | 7.17 (1.85) | 7.64 (1.81) | 7.99 (2.15) | # | 8.41 (1.71) | 8.72 (1.85) | 9.12 (2.75) | # |
| CRP (mg/L) | 0.33 (0.15, 0.66) | 0.27 (0.15, 1.00) | 0.27 (0.15, 0.74) | 0.82 (0.40, 1.59) | 0.95 (0.59, 2.02) | 0.99 (0.56, 1.81) | ||
| Smoker (%) | 47.0 | 57.1 | 30.3 | † | 5.6 | 1.8 | 8.1 | |
| IMT (mm) | 0.603 (0.060) | 0.632 (0.080) | 0.656±0.067 | **,§ | 0.651 (0.091) | 0.678 (0.083) | 0.709 (0.119) | **,§ |
Abbreviations and definition of the variables are the same as in table 1.
Values are expressed as mean (SD) or median (inter-quartile range) for continuous variables. §
p<0.05 between CCS 0 and CCS <10
p<0.01 between CCS 0 and CCS <10
p<0.05 between CCS <10 and CCS ≥10
p<0.01 between CCS <10 and CCS ≥10
p<0.05 for trend
p<0.01 for trend
The associations of IMT with risk factors were similar between the populations (Table 3). The category of IMT was significantly associated with age, BMI, BP, hypertension, and diabetes in both populations. Rates of hypertension were 21.0, 24.0, and 42.9 percent from the low to high tertile groups in the Japanese (p for trend <0.01), and 8.5, 13.0, and 20.0 percent, respectively, in the whites (p for trend 0.04). Rates of diabetes were 2.9, 3.1, and 12.1 percent from the low to high tertile groups in the Japanese (p for trend 0.03), and 0, 1.4, and 3.5 percent, respectively, in the whites (p for trend 0.12). There was no interaction between risk factors and populations in predicting the category of IMT.
Table 3.
Associations of intima-media thickness of the carotid artery (IMT) with risk factors in Japanese men aged 40–49 in Kusatsu, Shiga, Japan and white men aged 40–49 in Allegheny County, Pennsylvania, U.S. in 2002–2005
| Japanese |
Whites |
|||||||
|---|---|---|---|---|---|---|---|---|
| Category of IMT Number(%) |
Low (−0.598 ) 105 (42%) |
Middle (0.598–0.665) 96 (38%) |
High (0.665-) 49 (20%) |
P | Low (−0.598) 59 (24%) |
Middle (0.598–0.665 ) 69 (28%) |
High (0.665−) 115 (47%) |
P |
| Age (years) | 44.4 (2.8) | 45.3 (2.8) | 46.6 (2.4) | **,‡,§ | 44.1 (2.9) | 45.0 (2.7) | 45.6 (2.9) | **,§ |
| BMI (kg/m2) | 22.7 (2.7) | 24.2 (2.9) | 25.0 (3.6) | **,§ | 26.1 (3.0) | 28.2 (4.2) | 28.3 (4.4) | **,§ |
| SBP (mmHg) | 122.9 (15.7) | 124.3 (15.6) | 131.6 (18.0) | **,†,§ | 119.9 (9.7) | 122.3 (11.4) | 124.7 (11.6) | **,§ |
| DBP (mmHg) | 75.2 (11.8) | 75.8 (11.0) | 80.7 (13.3) | **,†,§ | 71.4 (7.0) | 73.4 (8.8) | 74.9 (8.9) | *,# |
| LDL-C (mmol/L) | 3.41 (0.93) | 3.49 (0.92) | 3.58 (0.90) | 3.34 (0.95) | 3.33 (0.84) | 3.66 (0.86) | *,‡,# | |
| HDL-C (mmol/L) | 1.45 (0.31) | 1.33 (0.33) | 1.35 (0.38) | 1.29 (0.36) | 1.20 (0.28) | 1.23 (0.34) | ||
| TG (mmol/L) | 1.51 (1.15, 1.98) | 1.60 (1.21, 2.03) | 1.50 (1.13, 2.19) | 1.21 (0.95, 1.86) | 1.45 (1.06, 2.00) | 1.46 (1.04, 2.11) | ||
| Glu (mmol/L) | 5.70±0.48 | 5.96 (1.15) | 6.09 (0.90) | *,# | 5.47 (0.43) | 5.55 (0.56) | 5.60 (0.75) | |
| Insulin (pmol/L) | 69.5±27.1 | 75.0 (35.4) | 72.2 (30.6) | 100.7 (60.4) | 110.4 (59.7) | 105.6 (56.9) | ||
| Fbg (umol/L) | 7.16±1.66 | 7.45 (2.17) | 7.37 (1.90) | 8.47 (1.69) | 8.65 (1.96) | 8.78 (2.31) | ||
| CRP (mg/L) | 0.27(0.15–0.51) | 0.43 (0.15, 0.90) | 0.29 (0.15, 0.72) | 0.80 (0.40, 1.91) | 0.87 (0.44, 1.88) | 0.92 (0.54, 1.56) | ||
| Smoker (%) | 53.3 | 42.7 | 53.1 | 6.8 | 4.3 | 5.2 | ||
| CCS >0 (%) | 22.9 | 27.4 | 48.2 | ‡,§ | 30.9 | 58.0 | 55.6 | **,§ |
| CCS ≥10 (%) | 6.0 | 8.3 | 25.3 | ‡,§ | 16.0 | 27.2 | 33.3 | § |
Abbreviations and definition of the variables are the same as in table 1.
Values are expressed as mean (SD) or median (inter-quartile range) for continuous variables.
p<0.05 between low and middle
p<0.01 between low and middle
p<0.05 between middle and high
p<0.01 between middle and high
p<0.05 for trend
p<0.01 for trend
The difference in the prevalence of CCS≥10 and mean IMT between the populations remained significant after adjusting for traditional risk factors (Model I in table 4), and further adjusting for CRP and fibrinogen (Model II), which were more favorable in the Japanese. Further adjusting for other factors did not attenuate the associations either (Model III). The difference in the prevalence of CCS>0, however, did not remain after adjusting for risk factors.
Table 4.
Multivariate-adjusted prevalence ratio for the presence of coronary calcium score (CCS) ≥10 and CCS>0 as well as multivariate-adjusted mean intima-media thickness of the carotid arteries (IMT) in Japanese men aged 40–49 in Kusatsu, Japan as compared to white men aged 40–49 in Allegheny County, U.S. in 2002–2005
| Prevalence ratio (95%CI) for CCS ≥10 in the Japanese compared to whites |
p | Prevalence ratio (95%CI) for CCS >0 in the Japanese compared to whites |
p | IMT (mean(SE)) | |||
|---|---|---|---|---|---|---|---|
| Japanese | Whites | p | |||||
| Crude | 0.52(0.35–0.76) | <0.01 | 0.68(0.55–0.85) | <0.01 | 0.616(0.005) | 0.672(0.005) | <0.01 |
| Model I | 0.51(0.31–0.83) | <0.01 | 0.94(0.71–1.25) | 0.67 | 0.622(0.006) | 0.666(0.006) | <0.01 |
| Model II | 0.52(0.32–0.85) | <0.01 | 0.95(0.71–1.27) | 0.74 | 0.621(0.006) | 0.667(0.007) | <0.01 |
| Model III | 0.53(0.31–0.92) | 0.02 | 0.98(0.71–1.36) | 0.91 | 0.623(0.006) | 0.665(0.007) | <0.01 |
Model I: Adjusted for age, body-mass index, systolic blood pressure, high-density-lipoprotein cholesterol, low-density-lipoprotein cholesterol, triglycer glucose, insulin, and pack-years.
Model II: Further adjusted for CRP and fibrinogen
Model III: Further adjusted for drinking, exercise, and medications for hypertension, diabetes, and hyperlipidemiai
A U-shaped association of ethanol consumption with coronary artery calcification was observed in both populations but that with IMT was not observed in either population. The odds ratio for the presence of CCS≥10 in light (−15 g of ethanol per day) or moderate (15–30 g of ethanol per day) alcohol drinkers as compared to non-alcohol drinkers was not significant in either population. In the Japanese, the odds ratios were 0.53 (95 percent CI, 0.17, 1.70, p=0.29) for light drinkers, 0.36 (95 percent CI, 0.07, 1.89, p=0.23) for moderate drinkers, and 1.24 (95 percent CI, 0.47, 3.32, p=0.67) for heavy drinkers (≥30 g of ethanol per day). In the whites, the odds ratios were 0.81 (95 percent CI, 0.38, 1.74, p=0.59), 1.01 (95 percent CI, 0.39, 2.63, p>0.75), and 1.11 (95 percent CI, 0.34, 3.62, p>0.75), respectively. The results were similar when the presence of coronary artery calcification was defined as CCS>0.
DISCUSSION
This population-based study shows that in men aged 40–49 the levels of subclinical atherosclerosis are lower in the Japanese than in whites. The evidence that levels of subclinical atherosclerosis evaluated by two different measures are lower in the Japanese supports the conclusion that in men aged 40–49 the Japanese have less atherosclerosis than whites. Our observation that in men aged 40–49 the Japanese had lower prevalence of coronary artery calcification is consistent with findings from the largest autopsy-based comparative study of atherosclerosis between the Japanese and Americans (13). To our knowledge, this is the first population-based study that compared subclinical atherosclerosis between Japanese and white men in the post-WWII birth cohort.
Our observation that similar risk factors were associated with coronary artery calcification in both populations indicates that similar risk factors are related to developing atherosclerosis in both populations. The observed associations of coronary artery calcification with risk factors in the whites are consistent with previous studies in whites in the U.S. (20, 21). Our observations are consistent with findings from autopsy studies showing that the levels of coronary artery atherosclerosis in young adults are associated with lipids, BP, and cigarette smoking both in Japan (22) and the U.S. (23, 24).
We observed an interaction between insulin and populations in predicting the category of CCS. Although the reason that in the Japanese levels of insulin in the category of CCS≥10 were significantly lower than those in the category of CCS<10 is not fully understood, one possibility is due to lower insulin secretion in the Japanese than in whites. A study reported that among subjects with impaired glucose tolerance (IGT), the insulin response in whites increases compared to that in those with normal glucose tolerance, whereas it decreases in the Japanese (25). Rates of those with IGT are likely to be much higher in those with the category of CCS≥10 than those with the category of CCS<10 both in the Japanese and the whites.
We observed no interaction between risk factors and populations in predicting the category of IMT. Although we observed significant linear associations of IMT with LDL-C only in the whites and with glucose only in the Japanese, the lack of the significant association of IMT with LDL-C in the Japanese and with glucose in the whites may be due to the small sample size.
Higher ethanol consumption in the Japanese did not explain the lower levels of subclinical atherosclerosis in the Japanese than in the whites. Some (26, 27), but not all (28, 29), epidemiological studies reported significant U-shaped associations of ethanol consumption with coronary artery calcification and IMT. We observed a U-shaped association of ethanol consumption with coronary artery calcification in both populations but the association was not significant in either population. We did not observe a U-shaped association of ethanol consumption with IMT in either population. Adjusting for ethanol consumption did not attenuate the differences in prevalence of coronary artery calcification or IMT (data not shown).
The lower levels of subclinical atherosclerosis in the Japanese are unlikely to be related to some lifestyle or genetic factors specific to Asian populations because decreasing trends in CHD mortality despite a rise in population levels of TC in Japan is unique among Asian countries. A recent review on lipids and CHD in Asia showed that CHD mortality in Asian countries increased with a concomitant rise in population levels of TC, except for Japan (30). In men in the post WWII birth cohort, i.e., men aged 35–44, CHD mortality increased during the 1980s through the 1990s in Korea, Taiwan (31) and Beijing, China (32), whereas it decreased in Japan (4, 31).
Our observations that levels of subclinical atherosclerosis remained significantly lower in the Japanese after adjusting for risk factors suggest that some factors other than those investigated here are related to the differences in the levels of subclinical atherosclerosis between the populations. The differences may be related to the difference in lifetime levels of obesity through adipocytokines or other factors (33), the levels of inflammation through some factors other than CRP (34), and the lipoprotein distributions (35). Genetic factors are unlikely to be primarily responsible for the lower subclinical atherosclerosis in the Japanese in Japan, given the substantial increase in CHD and IMT in migrant Japanese to the U.S. (15, 16, 36) and similar prevalence of coronary artery calcification between Japanese American and white men (37, 38).
Our observation that the prevalence of CCS>0 did not remain significant after adjusting for risk factors may suggest that the prevalence of coronary artery calcification defined as CCS>0 will become similar in the future between the populations if the Japanese keep a less favorable profile of many risk factors. We can not, however, deny the possibility that a low CCS, e.g., CCS<10, is an imaging artifact. In fact, among those with CCS>0 and CCS<10, 77.5 percent (38/49) in the Japanese and 69 percent (38/55) in the whites showed a very low CCS, i.e., CCS<5. Meanwhile, we re-read 42 randomly-selected scans of those with CCS<10 and the results were the same. In addition, both in the Japanese and the whites, a risk factor profile in those with CCS<10 was generally worse than a profile in those with CCS=0. Likewise, both in the Japanese and the whites, mean IMT was higher in those with CCS<10 than mean IMT in those with CCS=0 (Table 2). Follow-up study of those with a low CCS, therefore, is important.
The study has several limitations. The whites studied here may be healthier than the general white population based on the rate of cigarette smoking. If anything, however, this would make the finding that the Japanese have less subclinical atherosclerosis than whites more significant. Our observation that the Japanese had significantly higher prevalence of hypertension than the whites may not support our assumption that levels of BP have been similar between the populations throughout their lifetime. This would make the finding that the Japanese have less subclinical atherosclerosis than whites more significant. Our study included men and only those aged 40–49. We specifically focused on this specific sex- and age-group because, unlike older age groups, in this birth cohort TC and BP have been similar between Japanese and white men throughout their lifetime. It is possible that ethnic differences in prevalence of coronary artery calcification could be due to the differences in pathophysiology of coronary artery calcification (38, 39), and CCS might not reflect a real difference in atherosclerotic burden. Lower prevalence of both atherosclerosis and coronary artery calcification in the Japanese than in whites, however, is consistent with the data from the autopsy study (13) as well as patterns of CHD incidence and mortality (5, 12). In addition, we found lower IMT in the Japanese than in the white in this study. Although there was no interaction between risk factors and populations in predicting the category of either CCS or IMT except for insulin in predicting the category of CCS, this may be due to the small sample size.
In conclusion, we found that in men aged 40–49, levels of subclinical atherosclerosis evaluated as coronary artery calcification and IMT were significantly lower in the Japanese than in whites despite similar lifetime TC and BP levels and significantly higher rates of cigarette smoking in the Japanese. These associations remained significant after adjusting for traditional risk and other factors. The data may suggest there are some protective factors against atherosclerosis in the Japanese and warrant further investigations.
Acknowledgements
This research was supported by grants R01 HL68200 from the National Institutes of Health, B 16790335 and A 13307016 from the Japanese Ministry of Education, Culture, Sports, Science and Technology.
Footnotes
Conflict of interest: none declared.
REFERENCES
- 1.van den Hoogen PC, Feskens EJ, Nagelkerke NJ, Menotti A, Nissinen A, Kromhout D. The relation between blood pressure and mortality due to coronary heart disease among men in different parts of the world. Seven Countries Study Research Group. New England Journal of Medicine. 2000;342:1–8. doi: 10.1056/NEJM200001063420101. [DOI] [PubMed] [Google Scholar]
- 2.Ministry of Health and Welfare. National Nutrition Survey 1998. Tokyo: Daiichi Shuppan Publisher; 2000. [Google Scholar]
- 3.Ministry of Health Labor and Welfare. The fifth National Survey of Cardiovascular Diseases. Tokyo: Chuo Houki; 2003. [Google Scholar]
- 4.Okayama A, Ueshima H, Marmot M, Elliott P, Choudhury SR, Kita Y. Generational and Regional Differences in Trends of Mortality from Ischemic Heart Disease in Japan from 1969 to 1992. Am J Epidemiol. 2001;153:1191–1198. doi: 10.1093/aje/153.12.1191. [DOI] [PubMed] [Google Scholar]
- 5.Yoshida M, Kita Y, Nakamura Y, et al. Incidence of acute myocardial infarction in Takashima, Shiga, Japan. Circ J. 2005;69:404–408. doi: 10.1253/circj.69.404. [DOI] [PubMed] [Google Scholar]
- 6.Sekikawa A, Horiuchi BY, Edmundowicz D, et al. A "natural experiment" in cardiovascular epidemiology in the early 21st century. Heart (British Cardiac Society) 2003;89:255–257. doi: 10.1136/heart.89.3.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yano A, Ueshima H, Iida K, et al. Primary prevention of cardiovascular disease in youth (in Japanese) In: Komachi Y, editor. Trands in cardiovasucular disease. Tokyo: Hoken Dojin Sha; 1987. pp. 326–346. [Google Scholar]
- 8.Morrison JA, deGroot I, Edwards BK, et al. Plasma cholesterol and triglyceride levels in 6,775 school children, ages 6–17. Metabolism. 1977;26:1199–1211. doi: 10.1016/0026-0495(77)90112-3. [DOI] [PubMed] [Google Scholar]
- 9.Frerichs RR, Srinivasan SR, Webber LS, Berenson GR. Serum cholesterol and triglyceride levels in 3,446 children from a biracial community: the Bogalusa Heart Study. Circulation. 1976;54:302–309. doi: 10.1161/01.cir.54.2.302. [DOI] [PubMed] [Google Scholar]
- 10.Ueshima H, Kitada M, Iida M, et al. Serum total cholesterol, triglyceride level, and dietary intake in Japanese students aged 15 years. Am J Epidemiol. 1982;116:343–352. doi: 10.1093/oxfordjournals.aje.a113418. [DOI] [PubMed] [Google Scholar]
- 11.National Center for Health Statistics. Health, United States, 2004 With Chartbook on Trends in the Health of Americans. Hyattsville, Maryland: U.S. Department of Health and Human Services; 2004. [PubMed] [Google Scholar]
- 12.Sekikawa A, Satoh T, Hayakawa T, Ueshima H, Kuller LH. Coronary heart disease mortality among men aged 35–44 years by prefecture in Japan in 1995–1999 compared with that among white men aged 35–44 by state in the United States in 1995–1998: vital statistics data in recent birth cohort. Japanese Circulation Journal. 2001;65:887–892. doi: 10.1253/jcj.65.887. [DOI] [PubMed] [Google Scholar]
- 13.Takei H, Strong JP, Yutani C, Malcom GT. Comparison of coronary and aortic atherosclerosis in youth from Japan and the USA. Atherosclerosis. 2005;180:171–179. doi: 10.1016/j.atherosclerosis.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 14.Okamura T, Kadowaki T, Hayakawa T, Kita Y, Okayama A, Ueshima H. What cause of mortality can we predict by cholesterol screening in the Japanese general population? J Intern Med. 2003;253:169–180. doi: 10.1046/j.1365-2796.2003.01080.x. [DOI] [PubMed] [Google Scholar]
- 15.Robertson TL, Kato H, Rhoads GG, et al. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California. Incidence of myocardial infarction and death from coronary heart disease. Am J Cardiol. 1977;39:239–243. doi: 10.1016/s0002-9149(77)80197-5. [DOI] [PubMed] [Google Scholar]
- 16.Kagan A, Harris BR, Winkelstein W, Jr, et al. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California: demographic, physical, dietary and biochemical characteristics. Journal of Chronic Diseases. 1974;27:345–364. doi: 10.1016/0021-9681(74)90014-9. [DOI] [PubMed] [Google Scholar]
- 17.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. Journal of the American College of Cardiology. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 18.Thompson T, Sutton-Tyrrell K, Wildman R. Continuous quality assessment programs can improve carotid duplex scan quality. Journal of Vascular Technology. 2001;25:33–39. [Google Scholar]
- 19.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 20.Bild DE, Folsom AR, Lowe LP, et al. Prevalence and Correlates of Coronary Calcification in Black and White Young Adults : The Coronary Artery Risk Development in Young Adults (CARDIA) Study. Arterioscler Thromb Vasc Biol. 2001;21:852–857. doi: 10.1161/01.atv.21.5.852. [DOI] [PubMed] [Google Scholar]
- 21.Folsom AR, Evans G, Carr JJ, Stillman AE for the Atherosclerosis Risk in Communities Study I. Association of Traditional and Nontraditional Cardiovascular Risk Factors with Coronary Artery Calcification. Angiology. 2004;55:613–623. doi: 10.1177/00033197040550i602. [DOI] [PubMed] [Google Scholar]
- 22.Tanaka K, Masuda J, Imamura T, et al. A nation-wide study of atherosclerosis in infants, children and young adults in Japan. Atherosclerosis. 1988;72:143–156. doi: 10.1016/0021-9150(88)90075-5. [DOI] [PubMed] [Google Scholar]
- 23.McGill HC, Jr, McMahan CA. Determinants of atherosclerosis in the young. Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group. Am J Cardiol. 1998;82:30T–36T. doi: 10.1016/s0002-9149(98)00720-6. [DOI] [PubMed] [Google Scholar]
- 24.McGill HC, Jr, McMahan CA, Malcom GT, Oalmann MC, Strong JP. Effects of serum lipoproteins and smoking on atherosclerosis in young men and women. The PDAY Research Group. Pathobiological Determinants of Atherosclerosis in Youth. Arterioscler Thromb Vasc Biol. 1997;17:95–106. doi: 10.1161/01.atv.17.1.95. [DOI] [PubMed] [Google Scholar]
- 25.Fukushima M, Usami M, Ikeda M, et al. Insulin secretion and insulin sensitivity at different stages of glucose tolerance: a cross-sectional study of Japanese type 2 diabetes. Metabolism. 2004;53:831–835. doi: 10.1016/j.metabol.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 26.Vliegenthart R, Oei H-HS, van den Elzen APM, et al. Alcohol Consumption and Coronary Calcification in a General Population. Arch Intern Med. 2004;164:2355–2360. doi: 10.1001/archinte.164.21.2355. [DOI] [PubMed] [Google Scholar]
- 27.Mukamal KJ, Kronmal RA, Mittleman MA, et al. Alcohol Consumption and Carotid Atherosclerosis in Older Adults: The Cardiovascular Health Study. Arterioscler Thromb Vasc Biol. 2003;23:2252–2259. doi: 10.1161/01.ATV.0000101183.58453.39. [DOI] [PubMed] [Google Scholar]
- 28.Pletcher MJ, Varosy P, Kiefe CI, Lewis CE, Sidney S, Hulley SB. Alcohol Consumption, Binge Drinking, and Early Coronary Calcification: Findings from the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am. J. Epidemiol. 2005;161:423–433. doi: 10.1093/aje/kwi062. [DOI] [PubMed] [Google Scholar]
- 29.Demirovic J, Nabulsi A, Folsom A, et al. Alcohol consumption and ultrasonographically assessed carotid artery wall thickness and distensibility. The Atherosclerosis Risk in Communities (ARIC) Study Investigators. Circulation. 1993;88:2787–2793. doi: 10.1161/01.cir.88.6.2787. [DOI] [PubMed] [Google Scholar]
- 30.Khoo KL, Tan H, Liew YM, Deslypere JP, Janus E. Lipids and coronary heart disease in Asia. Atherosclerosis. 2003;169:1–10. doi: 10.1016/s0021-9150(03)00009-1. [DOI] [PubMed] [Google Scholar]
- 31.Sekikawa A, Kuller LH, Ueshima H, et al. Coronary heart disease mortality trends in men in the post World War II birth cohorts aged 35–44 in Japan, South Korea and Taiwan compared with the United States. Int J Epidemiol. 1999;28:1044–1049. doi: 10.1093/ije/28.6.1044. [DOI] [PubMed] [Google Scholar]
- 32.Critchley J, Liu J, Zhao D, Wei W, Capewell S. Explaining the Increase in Coronary Heart Disease Mortality in Beijing Between 1984 and 1999. Circulation. 2004;110:1236–1244. doi: 10.1161/01.CIR.0000140668.91896.AE. [DOI] [PubMed] [Google Scholar]
- 33.Matsuzawa Y. White adipose tissue and cardiovascular disease. Best Pract Res Clin Endocrinol Metab. 2005;19:637–647. doi: 10.1016/j.beem.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 34.Tiong AY, Brieger D. Inflammation and coronary artery disease. Am Heart J. 2005;150:11–18. doi: 10.1016/j.ahj.2004.12.019. [DOI] [PubMed] [Google Scholar]
- 35.Carmena R, Duriez P, Fruchart J-C. Atherogenic Lipoprotein Particles in Atherosclerosis. Circulation. 2004;109:III-2-7. doi: 10.1161/01.CIR.0000131511.50734.44. [DOI] [PubMed] [Google Scholar]
- 36.Watanabe H, Yamane K, Fujikawa R, Okubo M, Egusa G, Kohno N. Westernization of lifestyle markedly increases carotid intima-media wall thickness (IMT) in Japanese people. Atherosclerosis. 2003;166:67–72. doi: 10.1016/s0021-9150(02)00304-0. [DOI] [PubMed] [Google Scholar]
- 37.Curb JD, Masaki K, Liang S, et al. Association of traditional cardiovascular risk factors and coronary calcification in elderly Japanese-American men: the Honolulu Heart Program (Abstract: P234); 46th Annual Conference on Cardiovascualr Disease Epidemiology and Prevention; 2006. [Google Scholar]
- 38.Newman AB, Naydeck BL, Whittle J, Sutton-Tyrrell K, Edmundowicz D, Kuller LH. Racial Differences in Coronary Artery Calcification in Older Adults. Arterioscler Thromb Vasc Biol. 2002;22:424–430. doi: 10.1161/hq0302.105357. [DOI] [PubMed] [Google Scholar]
- 39.Bild DE, Detrano R, Peterson D, et al. Ethnic Differences in Coronary Calcification: The Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2005;111:1313–1320. doi: 10.1161/01.CIR.0000157730.94423.4B. [DOI] [PubMed] [Google Scholar]