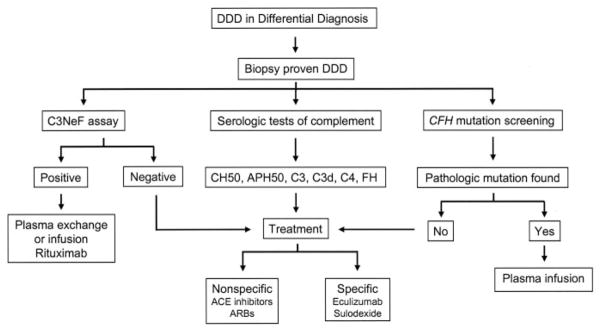
Figure 4.
Flow diagram illustrating the diagnostic evaluation and treatment of a patient with DDD. The diagnosis is made by renal biopsy. Serologic tests of complement should be obtained, C3NeF should be assayed, and CFH should be screened for mutations. In the presence of C3NeF, removal or dilution of the autoantibody should be considered via plasma exchange or infusion, and anti–B cell agents such as rituximab might be valuable. In the presence of pathologic mutations in CFH that lead to absent or dysfunctional factor H protein, plasma infusion should be considered (with the use of recombinant factor H in the future). In addition, nonspecific treatment should be aimed at controlling BP and proteinuria. Other treatments that should be considered include eculizumab (an anti-C5 antibody [see Figure 3]) and sulodexide (a heparanase inhibitor [see Figure 5]). The criterion for treatment success should be prevention of disease progression as determined by maintenance of or prevention of decrease in renal function. The secondary criterion should be normalization of activity levels of the alternative complement pathway as measured by C3/C3d ratios and C3NeF levels. After having reached a clinical steady state, reasonable follow-up steps could be monthly for the first 3 to 6 mo, every 2 mo for the rest of the first year, and subsequently every 6 mo, adjusting clinical monitoring if a flare in disease activity occurs.